Taylah MacDonell
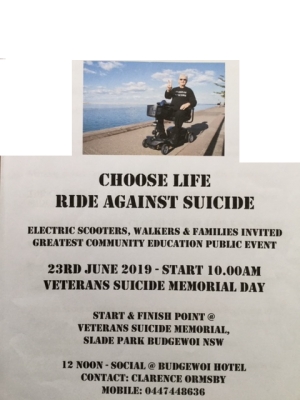
WALK AND RIDE AGAINST SUICIDE
WALK AGAINST SUICIDE
CHARITY - CENTRAL COAST COMMUNITY EDUCATION EVENT
Venue: Veterans Suicide Memorial Day, Slade Park, Budgewoi
Start and finish: North end Australia Rememberance Grove site
Date: Sunday 23rd June 2019 - families invited
BOOK IN: @ 9:20am with a start time of 10am.
Contact: Clarence Ormsby on 0447448636
AFOM 2018 Annual Report
A Mental Health Workshop for Parents/Carers of Adolescents
AFOM has collaborated with other organisations to present this workshop.
The workshop was organised as a result of community feedback from our Invisible Wounds Projects.
This is a topic that concerns so many, so this workshop will be a first step towards better understanding, education and knowledge of where to obtain help.

Self-Compassion Reduces Negative Mood Over Time
Nathan A Heflick Ph.D
New research shows that accepting negative moods can reduce them.

I am going to make a list. All I ask—indulge me, it's Christmas!—is that you decide whether these things make your life pleasant or unpleasant.
Without further ado, here is the list: Anxiety, Sadness, Shame, Guilt, Fear, Distress, Panic, Resentment, Anger.
Now, I doubt many of you were thinking, "Gee, these things sound fantastic. My life would be so much better if I could just feel a little more distress, shame, and resentment today." So what if there was a way to reduce the amount of these feelings you have in the future? Seems like a pretty good deal. But should people actively try and fight these emotional states or should they try and accept them?
New research headed by psychologist Brett Ford at the University of Toronto explored just this question. Specifically, it looked at if the amount that people "accept" their negative emotions is associated with (a) better mental health and (b) reduced negative moods over time. By acceptance, these authors do not mean simply allowing and being okay with negative things happening to you or being mistreated, but rather, experiencing and thinking about your own negative emotions in a non-judgemental way.
In one study of over 1,000 people, they found that accepting mental experiences was related to less anxiety and depression and to more life satisfaction. This was even when "controlling" for potentially related variables like cognitive re-appraisal (re-thinking something to make it more positive/less negative) and rumination. This means, basically, that the effect persisted even when those other variables were accounted for.
In Study 2, these researchers measured people's general level of acceptance of their negative thoughts and emotions. They then exposed participants in a laboratory to a variety of stressors. Participants with a higher level of general acceptance experienced lower levels of negative mood as a response.
In Study 3, they assessed around 200 participants over a six month period. They found that high levels of acceptance were associated with better mental health at Time 1, and the relationship between acceptance and positive mental health was explained by reduced levels of negative emotions six months later.
Taken together, these studies suggest that one way to reduce negative moods is to stop beating yourself up about thinking bad thoughts and having negative feelings. Accepting them—and this might be easier said than done but is still possible—can greatly improve your mental health.
It's no good to feel shame, anger, or distress, or any other negative emotion as a response to feeling poorly. Shaming yourself over shame, or making yourself distressed over your own anger, is likely to yield negative results.
In closing, I want to again make the point that accepting your mental states and your negative moods is not the same thing as accepting your life situations or allowing people to mistreat you.
Happy holidays, and I hope you all have a better year than the last!
References
Ford, B. Q., Lam, P., John, O. P., & Mauss, I. B. (2018). The psychological health benefits of accepting negative emotions and thoughts: Laboratory, diary, and longitudinal evidence. Journal of Personality and Social Psychology, 115(6), 1075-1092.
Understanding the Connection Between Sleep and Anxiety

Research findings suggesting that sleep loss and anxiety are closely linked were among those presented at Neuroscience 2018, the annual conference of the Society for Neuroscience held in San Diego, California. The news isn’t all dire, however—this year’s event offered some science-based encouragement along with causes for concern.
Neuroscience continues focusing on the mysteries of sleep (and yes, it’s still plenty mysterious despite its media ubiquity)—not only the perils of failing to get enough, but also the list of vital roles it plays in our brains.
Research discussed at this year’s event touched on a range of findings, from sleep's roles in memory consolidation to garbage removal in brain tissue. We’re learning via more studies each year that sleep, including well-placed naps, facilitates the brain’s consolidation of information—moving memory freight from short-term to long-term storage, and sharpening its accessibility for when we need it. Without sleep, memory simply doesn’t happen.
We’ve also learned that sleep provides the brain with an invaluable period of transporting toxins out of neural tissue through a complex garbage-removal system. Operating separately from the body's lymphatic system, the brain’s trash-disposal apparatus seems dependent on sleep to function properly. Links between neurodegenerative diseases like Alzheimer’s and the accumulation of toxins in brain tissue are exceptionally strong, and sleep loss is a likely culprit.
A panel session at this year’s event called “Threats of Sleep Deprivation” highlighted new findings on the connection between sleep loss and anxiety.
“Sleep deprivation isn’t what we usually think it is,” said session moderator Clifford Saper, MD, Ph.D., of Harvard Medical School. It’s usually not “staying up 40 hours all at once,” but rather gradually losing sleep over time.
Saper noted that most sleep deprivation is more specifically REM (rapid eye movement) deprivation, referring to the period of sleep during which the body becomes more relaxed while the brain becomes more active. During the normal cycle of sleep, people spend about 20 percent of the time in REM, but disrupted sleep derails the cycle, with consequences for memory, the nervous and immune systems, and more.
Research presented during the panel found that brain activity after periods of sleep deprivation mirrors brain activity indicative of anxiety disorders. The amygdala—seat of the brain’s fight or flight response—is particularly “aroused” when we haven’t slept enough.
One study found that the brains of participants who’d experienced even brief periods of sleep deprivation showed greater activity in a complex of “emotion-generating regions of the brain” and reduced activity in “emotion-regulating regions.”
These findings are linked to why people with anxiety disorders often report an explosion of anxiety first thing in the morning. Poor sleep seems to put the brain on-guard by triggering spikes in stress hormones like cortisol, producing an early a.m. “anxiety bloom” even before the day begins.
The panel also addressed the "vicious cycle of anxiety and sleep loss"—while sleep loss is often a precursor for anxiety disorders, anxiety also leads to sleep loss. The conditions fuel each other, with compounding effects.
Thankfully, science is also serving up some good news with practical applications. Because the link between anxiety and sleep is so strong, researchers reported that “sleep therapy” could be an effective method of treating anxiety disorders. Finding ways to improve an anxiety patient’s sleep could be one of the most overlooked and accessible treatment opportunities.
“The results [of the research] suggest that sleep therapy could reduce anxiety in non-clinical populations as well as people suffering from panic attacks, generalized anxiety disorder, post-traumatic stress disorder, and other conditions,” said panelist and lead study author Eti Ben-Simon, Ph.D., of the Center for Human Sleep Science at the University of California, Berkeley.
And the really good news is that many of the negative effects of sleep loss appear reversible after just one night of peaceful sleep.
“For healthy people, research shows that one night of recovery sleep brings systems back online and brings anxiety levels back to normal,” added Dr. Ben-Simon.
Which may help explain why previous research has found that catching up on sleep during the weekend turns out to be effective—a couple nights of solid sleep can balance many of the negatives from drudging through stressful weekday nights. It’s not an ideal solution (the gold standard is consistently sleeping well), but certainly better than not recovering at all.
The takeaway: even if you’re struggling to sleep well, make sure to at least get a recovery night or two during the week to tune down the emotion-generating parts of the brain and bring emotion-regulation back online. That’s just one among many benefits of getting a good night’s sleep, but an especially crucial one when it comes to managing anxiety.
Research discussed in this article was presented at Neuroscience 2018 the annual conference of the Society for Neuroscience. Research presented at the conference is generally considered preliminary prior to being published in peer-reviewed journals.
© David DiSalvo
Spring/Summer Newsletter

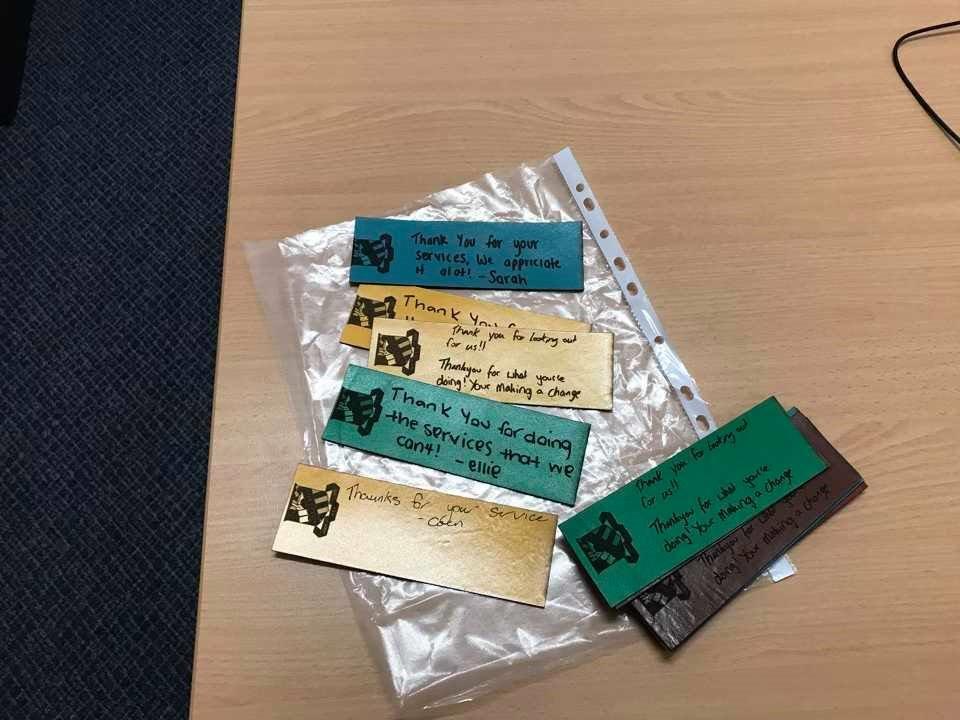
Everyone has been kept busy this last 12 months for all the board members. We would like to do some "Thank you" and "Congratulations" to just some of the people who have worked so hard this year.

Included with AFOM duties there has been lots of family changes and additions, hospitalisations, bushfires and family incidents for nearly all of us.
So AFOM would like to say thank you that despite all of things happening, you have hung in there and supported AFOM.
We had our 2017 AGM the day after our AFOM Fundraiser Dinner, which was a successful night, thanks to John, Ann and Belinda for organising it all.
Our Ambassador Linda Hurley was exceptional on the night, Linda had even written (and sung) a song for AFOM.
There was great fundraising – with the auctions and raffles.
Our 2018 AGM was a quieter affair, with lots of planning and business to attend to - and Subway wraps for lunch!
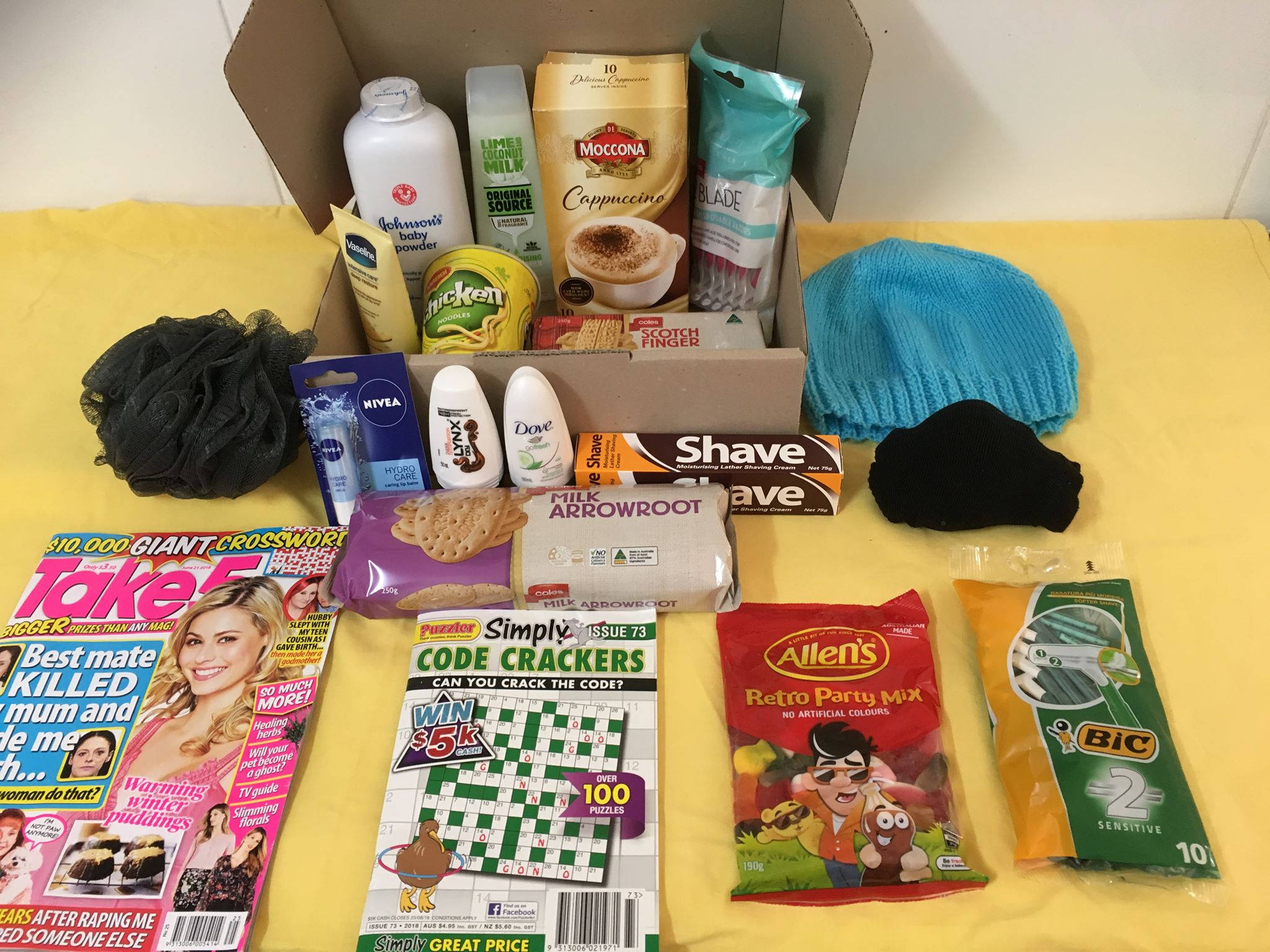
Belinda had a fundraiser to see Vivid – and the funds made from that trip- was used to pay for wool.
THANK YOU Belinda
A friend of AFOM (Ann Burns) is knitting a huge range of beanies, that went into the packages for the girls and boys overseas, using that wool, plus much of her own.
THANK YOU ANN!


We had some wonderful feedback from the different sections where the packages were delivered last Christmas. Belinda kindly offered her services to pack more this Christmas.She does an amazing job with it all. Cheryl and Vicki spent the day with her helping pack the right items into the right boxes. Job Well Done! THANK YOU Cheryl
THANK YOU Vicki
We did a small Social Media Campaign for donations. We did not want to impeded the donations and fundraising for Drought Effected Farmers. Year 7 Singleton High School did a volunteer drive for goods for the parcels with great success.
THANK YOU YEAR 7 Singleton High
Belinda and Co have also done an excellent job of organising Bunnings BBQ.
THANK YOU Belinda and CO. you people are amazing!
Ann and John continue to go to the Red Friday Coffee Mingle group, and John has run several Men’s Retreat at Boot Hill. Things are progressing there, with more Camp structures going up. The next Men's retreat may be held in January - stay tuned on our Facebook page for updates.


Because of time constraints The Women’s retreat was organised via a “Sister Group” Partners PTSD Support Group. The feedback from the retreat was excellent, however, I am not sure who went from this area – It was at the Gold Coast.
THANK YOU Donna Reggett and your group/s - you do amazing work.
Several other groups have run Fundraisers for AFOM in the previous 12 months – Masonic Lodge Singleton and Cessnock Lions Club.
THANK YOU Masonic Lodge Singleton and
THANK YOU Cessnock Lions Club
We finally have a PhD student that is using AFOM Prize Money. Her thesis is on Moral Injury. From the students notes:
My study is looking at the concept of moral injury - moral injury is a term that has been used for many years particularly in religious arenas, but has seldom been applied to those who witness or have to partake in events that are against their own moral fibre. This conflict results in dissonance that creates feelings of shame, guilt and self-condemnation - combined these can lead to suicide ideation, thoughts and attempt.
My study will be considered how moral injury relates to suicide in an Australian Defence Force context and will consider former members own narratives around their understanding and experience of moral injury.
Gail did a supporting document for the VVF to the Productivity Commission. The Productivity Commission contacted her to see if we wanted it to be put as a separate document. We had to make a decision rather quickly, but after some deliberation and emails with the VVF, we decided to leave it as a supporting document for the VVF. We felt (amongst other things) that a supporting document was more beneficial as a show of strength. Since that time the Productivity Commission has been in contact with Gail regarding issues around Families and Mental Health. They have asked her to review the draft report and to come down in the New Year to discuss some of the issues raised.
THANK YOU Graham Walker, for your help, input and connecting us up with the relevant people

Our own John went as a volunteer to the Invictus Games - a fantastic representative of AFOM. He reported back that it was an extremely rewarding experience and along the way made new connections for himself for future ventures.
THANK YOU John and Ann Bettley


We have been kept busy with issues raised by the community via our website- It is wonderful to have people around Australia that can assist people when they contact us. If you would like to be one of those people - please contact us - we can always do with more contacts in more places.
THANK YOU Jan Wallent
THANK YOU June Roe
THANK YOU Shelley Harboard
Another Board member - currently serving in the RAAF - Shaun McGill has just passed his Bachelor of Business - A huge congratulations to him and his family- Well Done!


Invisible Wounds:
AFOM have been asked if we could take over the registration and Programming of (1) Invisible Wounds Australia and (2) Invisible Wounds – PTSD Awareness, which the board has accepted.
Originally Set up and Run by the Girls in Western Australia (Partners of Veterans Australia WA Inc.) they have done an outstadning job including lobbying and successfully having a National PTSD Awarenss Day - The last Friday in May. AFOM hope to keep up the good work to your high standards.
THANK YOU


Further to that- the feedback from our previous Invisible Wounds has been to look at Adolescent Mental Health. We have been attempting for over 12 months to get the right people/forum to help run this workshop. Finally - we have a date April 3 2019.
This event will be slightly different format, and we are looking at having an expert panel to answer questions from the audience. As AFOM usually does, we looked and found that the gaps in education around Children and Adolescent Mental Health were the parents. So this is the major audience we will be catering to, however, we hope to have school teachers, carers, school counsellors as well.
footer
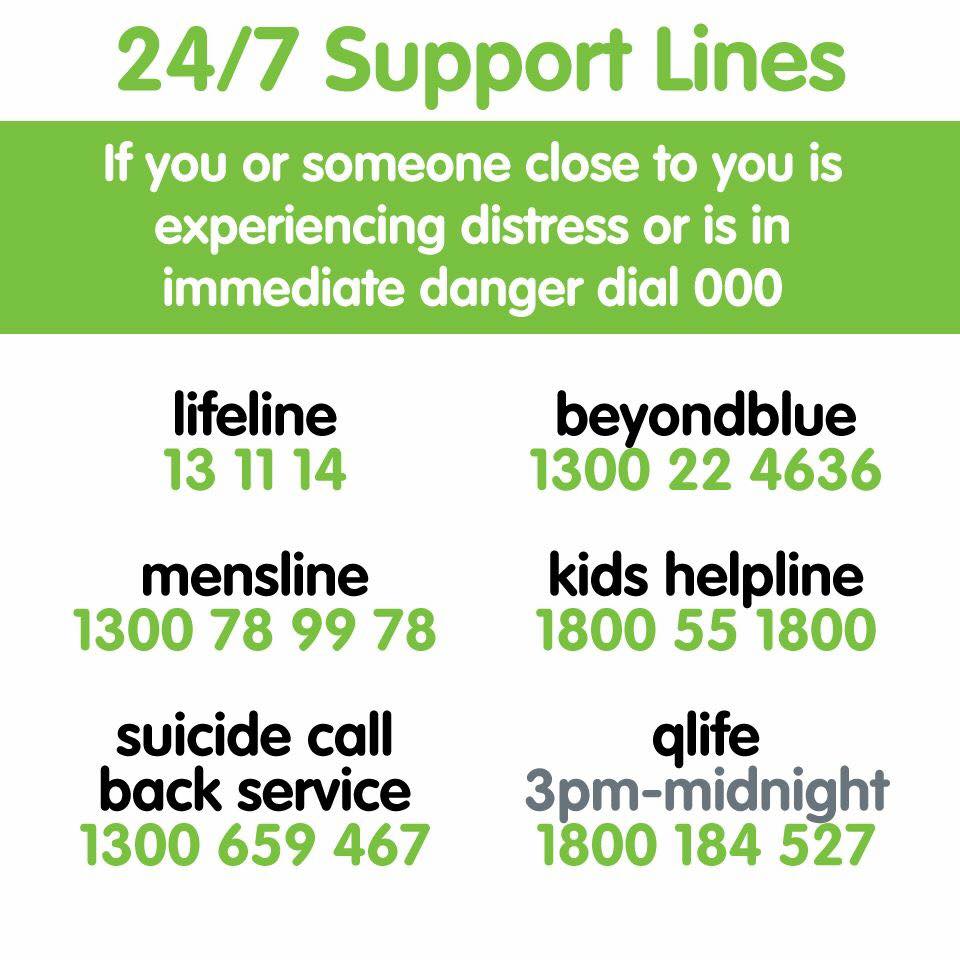
We at AFOM want to wish you all a safe and happy Christmas filled with Laughter and Joy and an even better 2019. If you are feeling the pressures that oftern occur, please know that we are here to help and we have put a list of numbers for organisations to call at the end of this newsletter -if they feel the need. Look after yourselves, your family, friends and neighbours, particularly this time of year.
The AFOM Team
PTSD in Women Returning From Combat: Future Directions in Research and Service Delivery
As of September 30, 2008 over 200,000 women were serving on active duty in the U.S. military, and women make up approximately 14% of deployed forces. While women are technically barred from serving in combat,they are serving in forward positions in greater numbers. Additionally, as of 2008, there were approximately 38,000 U.S. citizens serving as contractor personnel in Iraq– many of whom are women. These new role for women in military operations brings with it physical and mental health concerns, namely posttraumatic stress disorder or PTSD. PTSD affects approximately 2.6% of the U.S. population.Among military personnel serving in Operation Iraqi Freedom (OIF) and Operation Enduring Freedom (OEF), more than 17% percent of service members surveyed screened positive for PTSD.
Research has shown that there are significant sex differences in diagnosis and treatment of PTSD in the general public.However, much less is known about PTSD in women returning from combat. As the proportion of female veterans is projected to be 14% by the year 2010, it is critical that military, Department of Veterans Affairs (VA), and private sector providers are prepared to identify and care for the unique needs of female service members, veterans, and contractors with PTSD.
To assess the current state of the science, knowledge gaps, and research priorities on the issue, the Society for Women’s Health Researchconvened an expert workshop on December 8, 2008 in Washington, DC. Attendees discussed what is currently known about PTSD in women returning from combat and developed a roadmap for improving the diagnosis and treatment of PTSD in female service members. The following paper reflects a summary of the day’s discussions. It is not meant as a comprehensive review of the literature. A list of frequently used acronyms is available in Appendix I. Additional source information was used to supplement the discussion of the participants. References for these sources are given in the text.
Background – What is PTSD and What Are Its Causes
According the National Institute of Mental Health, PTSD is a condition that develops after a distressing ordeal that involved physical harm or the threat of physical harm. This harm may have happened to the person who develops PTSD or to a friend or loved one or may have simply been witnessed by the person who developed PTSD. People with PTSD may suffer flashbacks to the traumatic event, become aggressive or withdrawn, have nightmares, and become emotionally numb or even violent. Symptoms of PTSD usually appear about three months after the traumatic event. PTSD generally affects twice as many women as men, and women with PTSD report having a lower quality of life than do men with PTSD. The time to remission of PTSD symptoms is longer in women than in men, and the rate of remission in women is half that
- This workshop was cosponsored by the National Institute of Mental Health, DynCorp International, and Magellan Health Services in men.For more information regarding criteria for diagnosing PTSD, please refer to Figure I. For a discussion of the neurobiological pathways of PTSD, please refer to Appendix II.
What Causes Sex Differences in PTSD?
Workshop participants engaged in a detailed discussion of potential causes of sex differences in PTSD. Participants noted that animal models have shown that male and female rats process stress differently. They also noted that male rats tend to develop more acute reactions (i.e., they can respond quicker) to stressors while females exhibit greater object memory after a traumatic event, meaning they learn to recognize stressors in the future. While these behaviors may pose evolutionary advantages for each sex, in humans they lead to women “holding onto” negative memories more so than men, causing women to “relive” the traumatic event more than their male counterparts. Participants also shared that in general, males also exhibit a faulty memory during times of high stress, possibly protecting them from PTSD. Women react more negatively than men to interpersonal stressors and laboratory stressors. Women also show more ruminative coping. In general women have greater frequency and intensity of negative emotions. Women have more startle modulation and autonomic responses to aversive content – all of which can make women more susceptible to developing PTSD.
Workshop participants also theorized that sex difference in the hypothalamic-pituitary-adrenal (HPA) axis, a major part of the neuroendocrine system that controls reactions to stress and regulates many body processes, may also contribute to disproportionate rates of PTSD in women and men.
Figure I. Criteria used for diagnosing PTSD†
Criterion A1: A person is exposed to a life-threatening event either directly or through an experience happening to someone significant to him or her.
Criterion A2: The event results in an intense, overwhelming sense of fear or horror or the person becomes disorganized in their response to the trauma. This reflects a neurobiological response to stress. Men generally have a greater number of A1 events, while women have a greater overall exposure to both A1 exposures and A2 symptoms.
Criterion B: Re-experiencing the traumatic event. characterized by five symptoms: 1) recurrent, intrusive, distressing recollections including thoughts, images, and perceptions; 2) recurrent, distressing dreams; 3) acting or feeling as if the traumatic event were recurring (reliving, illusions, hallucinations, dissociative flashbacks); 4) experiencing psychological distress at exposure to internal or external reminders or cues; and 5) a physiologic reactivity at exposure to cues.
Criterion C: Symptoms of avoidance. These symptoms can manifest as avoiding thoughts, feelings, conversations, people, activities, or places related to the traumatic event. Persons exhibiting avoidance may also experience partial or total memory loss surrounding the traumatic event. The individual may also suffer from diminished interest in important activities or feel detached or estranged from others. They may also have a limited range of affect, meaning they are unable to experience loving feelings. They may also exhibit a foreshortened sense of future, e.g., one doesn’t expect to have a career, marriage, or normal lifespan.
Criterion D: Persistent symptoms of increased arousal. These symptoms of arousal (e.g., difficulty falling or staying asleep, irritability or outbursts of anger, difficulty concentrating, hyper-vigilance, and exaggerated startle response) were not present prior to the traumatic event.
Criterion E: The symptoms of criteria A, B, C and D must be present for at least one month.
Criterion F: The above symptoms must result in significant distress or impairment in social, occupational, or other important areas of functioning.
†From the Diagnostic and statistical manual of mental disorders DSM- IV-TR, Fourth Edition. American Psychiatric Association; 2000.
The HPA axis plays a major role in the body’s reaction to stress. A study by Uhart et al. found that men have a greater HPA axis response to psychological stressors than women while females have greater hormonal reactivity to chemical stressors such as naloxone. More research is needed into these sex differences as they relate to the development and treatment of PTSD.
Sex and Gender Issues in Combat-Related PTSD
In considering the diagnosis, prevention, and treatment of PTSD, workshop participants noted that there are unique issues facing female active military personnel, veterans, and other women returning from combat. They are affected by a number of trauma-related conditions, including, but not limited to, PTSD, traumatic grief, unexplained somatic symptoms, depression, sleep disturbances, increased use of tobacco and alcohol, and increased family violence and conflict. A 2004 study found that returning OIF/OEF service members were significantly more likely to suffer from mental health problems, including PSTD, than those not exposed to combat. Of those reporting mental health issues, only 20-40% sought medical care. Perceived barriers to care included fear of stigmatization, lack of trust in the medical system, and lack of knowledge of how to access care. A study that estimated prevalence in the entire deployed force as of 2007 showed that the number of combat traumas experienced while deployed was the single best predictor of PTSD as well as of major depressive disorder (MDD), and that only half of those with a probable current disorder had sought any mental health treatment in the prior year. Perceived barriers to care included concerns about the effectiveness of treatment as well as institutional barriers such as lack of confidentiality and potential harm to the military career.
Traumatic brain injury is another contributing factor to PTSD in men and women returning from combat. A 2008 study of combat service members found that almost half of service members suffering from mild traumatic brain injuries also met the criteria for PTSD. Because diagnostic techniques and evidence-based treatment protocols for post-concussive symptoms for combat- related head injuries are lacking,more research is needed into the appropriate diagnosis and treatment of PTSD in service members with traumatic brain injury.
PTSD and Females Military Personnel
Because the female facing combat conditions is a relatively new phenomenon, little is known about the unique needs and issues facing the female service member and other women with combat-related PTSD. Workshop participants discussed a recent, informal survey of health care providers at Walter Reed Army Medical Hospital and Bethesda Naval Hospital that found that approximately 13% of active duty patients with PTSD were women.Of the responding clinicians, 35% stated that their female patients reported more depressive symptoms than did their male patients. Male patients reported more irritability and anger, nightmares, and flashbacks. The responding clinicians also stated female patients are more receptive to psychotherapy while men expressed a stronger preference for medication. An important sex difference in PTSD in combat troops is that almost 65% of the respondents said that sexual trauma (either childhood or in theater) was an in issue in the treatment of their female patients with PTSD. No respondents cited sexual trauma as an issue for male patients. For men, the traumatic event was related to killing or seeing people killed or injured.Workshop participants shared that army medical data demonstrate that about 11% of identified cases of PTSD from OIF/OEF are in females, which is similar to the proportions of women serving in those theaters.
Treatment of Combat-Related PTSD
Of interest to the workshop participants were possible new treatment modalities for PTSD. Discussion centered on the role of allopregnanolone (ALLO), a neurotransmitter that mediates the fear response, in the treatment of PTSD. The same enzyme that makes ALLO also converts testosterone to its inactive form. Studies in military trainees have demonstrated that testosterone levels actually fall during the military’s Survival, Evasion, Resistance, and Escape (SERE) training. Workshop participants remarked that when testosterone levels fall, ALLO is reduced, resulting in increased stress and aggression. This aggression can be blocked with the use of a class of antidepressants known as selective serotonin reuptake inhibitors (SSRIs), which normalize the brain’s ALLO levels. However, for individuals who do not respond to SSRIs, which is at least 50% of women in treatment studies, participants theorized that it is possible that a more effective medication would be ganaxalone, a synthetic form of ALLO, which has been shown to prevent fear conditioning and anxiety.
Progesterone may be another treatment modality for women with PTSD. As stated earlier, progesterone is a precursor of ALLO. Levels of progesterone fluctuate with a woman’s menstrual cycle and pregnancy. Higher levels of progesterone in the luteal phase of the menstrual cycle are associated with higher levels of ALLO and a suppression of the HPA and autonomic responses to stress. Workshop participants theorized that women on steroidal birth control might be at a higher risk for developing PTSD as they do not generally experience a luteal phase during their menstrual cycles. Participants agreed that more research is needed into the use of progesterone in the prevention and/or treatment of PTSD.
Dehydroepiandrosterone (DHEA), a precursor of the sex steroids, is another possible avenue of treatment for PTSD. Studies of DHEA in animals have shown DHEA to increase ALLO and decrease cortisol levels.Levels of dehydroepiandrosterone sulfate (DHEAS), the storage form of DHEA, are 50-70% lower in women.During the second half of the menstrual cycle, women metabolize DHEA faster than men, possibly resulting in lower levels of DHEA and leaving women more susceptible to PTSD.
Workshop participants also discussed sex differences in the role of catecholamines in memory retention as catecholamines seem to play a larger role in women’s memory retention as compared to men. High levels of catecholamines during stress promote the consolidation of emotionally significant memories.Beta-blockers such as propranolol, which prevent memory reconsolidation, are frequently given to patients who were exposed to traumatic events to prevent the development of PTSD. However, a recent study of OIF/OEF service members returning home with burn injuries found that propranolol did not prevent PTSD in burn patients. But, this study did not take into account any psychological counseling that may have been received or when that counseling may have occurred in relation to the propranolol administration. The authors concluded that the timing of propranolol administration and psychological counseling resulting in memory reactivation needs further investigation.
Lastly, workshops participants also discussed the potential role of neuropeptide-Y (NPY) in the treatment of PTSD. At high levels of stress, NPY makes norepinepherine more effective. In men with PTSD, levels of NPY are extremely low. Combat troops exposed to stress have been found to have lower levels of NPY. Normalizing the levels of NPY may improve the resiliency of the brain to the effects of trauma.
SSRIs have shown a positive effect in treating non-combat related PTSD. However, in combat-related PTSD, SSRIs were found to be ineffective.Workshop participants remarked that existing research on combat-related PTSD has been conducted primarily on men, and more research is needed to gauge the potential efficacy of SSRIs for women with combat-related PTSD. Research is also needed on the effectiveness of non-SSRI antidepressants for combat- related PTSD.
Cognitive processing therapy (CPT), which includes both cognitive and exposure components, is one of the more effective treatments for PTSD. CPT focuses not only on anxiety resulting from trauma, but also on a range of emotions including shame, sadness, and anger. Based on the results of a 2007 study published in the Journal of the American Medical Association, the VA is currently implementing a program of prolonged exposure therapy (a form of cognitive processing therapy to treat PTSD in female service members). The 2007 found that prolonged exposure therapy was effective in treating PTSD in female veterans and active duty personnel.
Cognitive processing therapy and exposure-therapy have shown promise in treating both combat and non-combat related PTSD. As the military and VA implement more programs to treat PTSD in female military personnel, resulting data will help to strengthen and refine the existing knowledge base regarding treatment guidelines.
Other Mental Health Issues Unique to Women in Combat Situations
Workshop participants discussed the fact that while all service members face stress when deployed to a combat area, female service members face unique stressors that may impact their mental health. Participants noted that serving in the military and/or as a military contractor is an atypical career path for women. As such, women in the military may experience feelings of isolation and lack of support from colleagues, friends, and family. Women also bear the stress of often being the primary caregiver for family members – not only for their children, but also for their aging parents. The stress of extended deployments for these women is compounded by the demands of caring for their families back home. Participants also remarked that the lack of adequate and safe hygiene facilities for women in combat can lead to both physical and mental health issues. For example, a lack of adequate facilities for urination can lead to an increase in bladder infection. As many latrines are somewhat isolated, women also face a threat (either real or perceived) to their personal safety when faced with the need to urinate. Stressors such as these can contribute to, compound, and/or complicate the diagnosis and treatment of PTSD in women.
Prevention and Treatment of PTSD in Theater
When a service member or contractor is diagnosed with PTSD, is it better for her to be medically discharged or to be treated in theater and returned to duty? Participants noted that when service members are discharged, they lose the support and structure of steady employment. According to workshop participants, the military has recognized that PTSD and mental health are significant issues for combat troops and has deployed over 200 mental health providers to Iraq. The purpose of these providers is to prevent mental health disorders, as well as to treat and restore affected service members to active duty. In 2006, the Department of Defense issued guidelines for deployment and continued service for military personnel who are suffering from psychiatric disorders or who are prescribed psychiatric medications.These guidelines allow for the use of SSRIs and other psychiatric medications in theater when appropriate, but codify the prohibition against the use of other psychiatric medications such as lithium and antipsychotics. The military has also developed web-based programs to help service members cope with the stressors of deployment and combat.
Despite these efforts, the military still faces significant challenges to providing appropriate mental health services to service personnel. Workshop participants identified these challenges as including a growing population of service members suffering from PTSD, a shortage or trained providers, multiple deployments, and traumatic brain injury. Upon being released from active duty, service members access services through the VA or private providers. More research is needed on how to best provide mental health services to both active duty personnel and veterans. There is ongoing research in VA on the provision of mental health services, and also on screening for PTSD. The military has also implemented various programs aimed at better screening. Workshop participants noted that there might be a need to collaborate with the private sector to improve the screening on veterans in the private health care sector.
Workshop participants also noted that consultants and military contractors exposed to combat situations face similar challenges and barriers to obtaining appropriate services to diagnose and treat PTSD. More research is needed to assess what services are available to these women, both in theater and when they return home.
Military Sexual Trauma and PTSD
Aside from trauma directly related to combat experiences, female service members face the risk of military sexual trauma (MST), the term that the Department of Veterans Affairs uses to refer to experiences of sexual assault or severe, repeated sexual harassment experienced during military service. As noted by workshop participants, MST is not a uniquely female problem. While the percentages differ, the absolute numbers for veterans – male and female – who have suffered MST are fairly comparable. Gender responses to MST may differ, and research in ongoing regarding this issue. According to the National Center for PTSD, there is almost no empirical data comparing MST to sexual trauma that occurs outside of military service, although there is anecdotal evidence the MST is unique from and has quantitative and qualitative psychological outcomes.
In a 2005 study of Gulf War veterans, Kang et al. found that exposure to sexual assault during deployment conferred a greater risk of developing PTSD than did combat exposure.In 2002, approximately 3% of active duty military women and 1% active duty military men experienced sexual assault.A more recent report found that 6.8% of active duty women and 1.8% of men reported unwanted sexual contact.New screening programs can detect MST and facilitate access to mental health services for both male and female victims of MST, thereby mitigating the burden of psychiatric illness for these service personnel.Workshop participants praised the VA for being proactive in addressing MST by mandating universal screening of all veterans for a history of MST. According to workshop participants, each VA facility has identified a Military Sexual Trauma Coordinator to oversee the screening and treatment referral process.
New Systems of Care for Combat-Related PTSD
A study published in 2004 found that for those Iraq war returnees who screened positive for a moderate to severe mental health disorder and wished to receive help for those services, only 23- 40% reported receiving professional help in the preceding 12 months. A more recent survey found that only 53% of military personnel with a probable diagnosis of PTSD had sought care in the previous year. Of those who sought care, just over half received minimally adequate care. In 2007 the military launched RESPECT-Mil (Re-engineering Systems of the Primary Care Treatment (of depression and PTSD) in the Military) to improve access to mental health services for those military personnel suffering from PTSD and depression. The program involves routine screening for PTSD and depression during all primary care visits, assessing all those who screen positive for depression and PTSD, referrals to appropriate treatment, and care coordination and follow-up by primary care providers.This program may be particularly effective for identifying and treating PTSD in female service members and veterans since women are more likely than men to report problems to and seek help from their primary care providers.The VA and military are also exploring other avenues of treating PTSD. An internet-based, therapist-assisted self-management program for PTSD has shown promise as a means to deliver effective treatment to service personnel.
The VA system will be an invaluable source of mental health services for women returning from deployment. Currently, 12%, or more than 45,000, of the total number of OEF/OIF veterans using VA services are women. Workshop participants noted that female veterans may be more likely to use VA care than are their male counterparts, but that women may be less likely then men to report PTSD symptoms in a VA setting. Participants noted that women are more likely to report depression and general anxiety symptoms and are twice as likely to be diagnosed with personality disorders. Workshop participants praised the VA for being a leader in its efforts to care for the female veteran, citing the VA’s appointment of a full-time Women Veterans Program Manager at every VA facility and a Women’s Health Science Division in the National Center for PTSD as examples of its leadership. They also discussed the need for the VA to develop more gender-sensitive programs for diagnosing and treating PTSD in female veterans.
Diagnosing and Treating Combat-Related PTSD in the Private Sector
Once a female service member becomes a veteran or a contractor/consultant returns home, new problems accessing services for PTSD can arise. Since PTSD symptoms do not generally manifest until three to six months after a traumatic event,7 many women may leave the military without a diagnosis of PTSD in their medical charts. Workshop participants stated that upon leaving active duty, many women, especially those who were/are reservists, may receive their healthcare through the private sector. Participants noted that veteran status is not generally ascertained in most health plan and employer eligibility files. Without an adequate history of veteran status, providers may not screen for combat-related disorders. Further complicating the delivery of services for women is that even if the provider knows a patient’s veteran status, there is a misperception about women’s roles in the military – that women are not directly exposed to combat situations. As such, PTSD symptoms may go unrecognized or be misdiagnosed. Private sector providers not familiar with the treatment of PTSD may mistakenly prescribe drugs such as benzodiazepines for symptom management, despite the fact that benzodiazepines have not been shown to be effective in treating PTSD.42 Workshop participants cited a concern that when private sector physicians do recognize PTSD symptoms in their patients, they may not be familiar with the VA and available services for PTSD. Further, there is a financial disincentive to the physician for referring patients to the VA for care.
Participants discussed the opportunities for the private sector to improve the diagnosis and treatment of combat-related PTSD. For example, during this workshop, Magellan Health Systems presented information about its CME programs promoting evidence-based practices guidelines for diagnosing and treating PTSD. These training programs include modules on military cultural competence and meeting the mental health needs of returning veterans.43 Further research is needed into developing appropriate screening and treatment of PTSD for service members returning from combat and reentering into the private sector.
Summary: Developing a Research Agenda and Improving Patient Care: What Health Care Professionals Need to Know
As the above report states, there are multiple areas in which our knowledge of PTSD in female service personnel is lacking. Most research models for PTSD were built around men. These models will need to be reexamined and redesigned to better target women. In the field of psychobiology, there is a need to look for new models for high stress populations in which there are a greater proportion of women (e.g., competitive athletes, law enforcement personnel) as an approach to supplement our limited knowledge of sex differences in the development of PTSD. Additionally, while research has been examining the role of sex hormones (estrogen in women and testosterone in men) in the development of PTSD, researchers should also look at the effects of androgens in women and estrogen in men.
Genetics may also play a significant role in the development of PTSD. More research is needed into the effects of polymorphisms in ethnic groups, as well as the effects of polymorphism on the effectiveness of medications and cognitive approaches to treating PTSD. In order to facilitate genetic studies, the Department of Defense and the VA will need to coordinate efforts and facilitate the implementation of research networks across facilities.
The military furthers our knowledge about combat-related PTSD in women by developing command awareness of the importance of medical studies to promote participation by their troops. Recruitment into research studies will be especially important for women as this will be the first time we will be observing the effects of combat on a large number of female service members. As the military begins to draw down from its current theaters of combat and women are released from active duty, it is important that we track how they are discharged and with what medical appointments or treatment referrals.
As women are returning from combat to their families, we will need to examine the effects of women’s PTSD on families. Additionally, women are at high risk for divorce and domestic violence when men return from combat. Will we be seeing the same for men who have stayed home while their spouses were deployed? Questions to ask include the following:
-
How do women react when they return post-deployment?
-
How do they treat their spouses, and/or children?
-
How do we instill health promotion behaviors early in the separation process and not wait
until post-deployment?
-
What are the effects of PTSD on parenting and children’s mental health?
Researchers need a better understanding of the natural course of PTSD over the lifecourse. Further, we know little about the effect of multiple deployments on women over time. For example, we know that former military men with PTSD are at higher risk for substance abuse. We do not yet know if women develop co-morbid substance abuse problems at the same rate as their male counterparts. A focus on sex differences in treatment and outcomes measurements is needed to better understand the needs of female service personnel.
Ideally we would like to prevent PTSD in our combat troops. Until effective prevention strategies are developed, the best the military can do is to train healthcare professionals in identifying early symptoms of PTSD so that those displaying such symptoms can receive early intervention. As cumulative trauma can significantly increase one’s risk for developing PTSD, military healthcare providers will need to be especially cognizant of service members’ prior exposure to combat and other stressors, whether though multiple deployments or service members’ experiences prior to enlistment.
Within the military system, military leaders should talk to their troops about the importance of seeking help for mental health disorders. The language and attitudes of commanders can significantly impact a service member’s willingness to seek and comply with mental health treatment. Service members need to be able to believe that getting mental health care won’t impact their career.
In the private sector, clinicians first and foremost need to know a woman’s military status. As stated earlier, clinicians in the private sector do not routinely screen for military service. Training must be provided to primary care physicians including OB/GYNs, to help them identify potential cases of PTSD in their female patients and to assist them in making informed referrals for these patients. Possible avenues for such training programs include health plans and medical professional societies. Additionally, models for collaboration between private sector and VA providers need to be developed to overcome private sector physicians’ fear of ‘losing’ patients to the VA system.
Private sector clinicians need more and better tools for opening a dialog about PTSD with their female patients. Posters about the signs and symptoms of PTSD could be posted in waiting rooms or restrooms of clinics. These posters could trigger a discussion of symptoms between patient and provider. Clinicians need better and more appropriate screening tools, as well as access to suitable resources if a patient does screen positive for PTSD.
All clinicians need to have a better understanding of the role of co-morbidities as they relate to PTSD. In the absence of better screening tools for PTSD, co-morbidities such as alcohol and substance abuse, irritable bowel syndrome, and migraines may signal an underlying case of PTSD. We need to develop effective working relationships across systems at the state, federal, and local, as well as across the military and private sector. A better electronic infrastructure is essential for sharing medical records across these systems. The Departments of Defense and Veterans Affairs, as well as the private sector, have been working on such systems for some time. Attention should now be focused on making those systems work across agencies and public/private sectors.
Taken from - A Report by the Society for Womens Health Research. Link to paper with full refrences - https://swhr.org/wp-content/uploads/2014/07/PTSD_in_Women_Returning_From_Combat-reduced_file_size.pdf
Combat-related PTSD calmed by yoga therapy

For thousands of years, yoga has been used to calm both mind and body.
Now, clinical yoga therapy has been found to alleviate the symptoms of chronic combat-related post-traumatic stress disorder (PTSD), potentially providing a treatment to deliver much-needed relief for the hundreds of military veterans in Australia suffering from the debilitating condition.
In a dynamic industry partnership, the research from the
Repatriation General Hospital, the University of South Australia and Mindful Movement Physiotherapy, reveals across-the-board improvements for PTSD sufferers, including reduced stress, depression and anxiety.
Lead researcher, Senior Psychiatrist and Director of the PTSD Unit at the Repatriation General Hospital, Dr Linda McCarthy says the Australian-first study confirms the clinical utility of yoga as an adjuvant strategy for combat-related PTSD.
“Combat-related PTSD is the one of the most common mental health conditions impacting veterans and their families, representing 15 per cent of claims through the Department of Veteran’s Affairs,” Dr McCarthy says.
“Following the yoga intervention, 64 per cent of veterans in the study scored less than the diagnostic cut-off point for PTSD, with their average scores being nearly 10 per cent below the lower limit.
“And 85 per cent of participants showed decreased scores on the PTSD assessment tools; both clearly indicating the positive effects of yoga as a treatment for PTSD.”
The research used a range of clinical assessment tools and biomarkers to track the responses of 30 Vietnam veterans as they participated in a series of eight weekly trauma sensitive yoga sessions, each lasting 90 minutes.
“By providing yoga as a treatment therapy, we’ve been able to clinically reduce the markers of depression, anxiety and stress among military veterans. This has also extended to improvement in their sleep quality and quality of life scores,” Dr McCarthy says.
Lead research consultant, UniSA’s Associate Professor Chris Alderman says that the relative scarcity of effective treatment options for managing chronic PTSD presents a strong case for the exploration of alternative therapies.
“While psychological interventions and pharmacological treatments exist to treat PTSD, these are often labor intensive and are associated with adverse side effects,” Prof Alderman says.
“The research gives us reason to be optimistic about this as a new treatment strategy for sufferers of PTSD, with proven positive health benefits.
“Now we need to undertake further research into yoga as a potential treatment method for combat-related PTSD.
“As we prepare to mark Remembrance Day this weekend, the positive results of new approaches to this important issue are something to celebrate and embrace.”
Notes for editors
Diagnostic measures used to diagnose PTSD, include: the PTSD checklist (PCL), the Depression, Anxiety and Stress Scale (DASS), the Pittsburgh Sleep Quality Index (PSQI), the Adult/Adolescent Sensory Profile, and the SF36 Quality of Life Instrument.
Media contact: Annabel Mansfield mobile: 0417 717 504 email: This email address is being protected from spambots. You need JavaScript enabled to view it.
Mens Retreat - More info to come!
Heads up! - We are holding another mens retreat.

Want to get away for a couple of days and enjoy a men’s only camping weekend? Then this is for you!
For current and past serving military and front line responders: police, firemen, ambulance officers etc.
Dates: 6th June till 10th June 2018
Costs of this event is to come, this is just a heads up to clear your schedule
For more information, contact John to 0404836765 or This email address is being protected from spambots. You need JavaScript enabled to view it.